Healthcare costs are a mystery in the United States. Questions my patients and I (as a patient) always ask — is this provider in-network? what’s the copay for this provider? is there a different copay for this procedure? what’s the co-insurance? where am I with my max out-of-pocket (OOP)? does this count towards my OOP? The questions are endless. The transparency is non-existent.
When it comes to lactation consulting coverage, there is good news and bad. Let me start with the bad so that I can later bring you back with the good =).
The bad…
- Most insurance companies have no or very few independent lactation consultants in-network
- Most insurance companies don’t know how to deal with charges from a lactation consultant
- Most insurance companies (even the ones that pay for services) do not cover travel fees
The good…
- All (mostly) insurance companies have some kind of lactation consulting benefits
- The Affordable Care Act mandates that insurance companies pay for breastfeeding support before and after birth (https://www.healthcare.gov/coverage/breast-feeding-benefits/) — there is an exception for grandfathered, or older and not-updated, plans
- Breastfeeding support is part of women’s preventive health services so it is NOT subject to cost-sharing – this means, in most cases, you should not be paying a copayment, deductible, co-insurance or anything else for the services. Your insurance company should either pay full contracted rates with in-network providers or if they are not able to provide in-network help, they have to pay the fees of the out-of-network providers.
That said – here’s a quick guide to ensure you maximize your lactation consulting benefits:
- Call or access the online provider registry to see if you have in-network lactation consultants (IBCLCs, CLCs):
A. If there are many providers listed, your insurance plan is likely “breastfeeding friendly.” You should have no problem finding someone who will see you and submit a bill on your behalf without charging you at the time of service. These providers will submit a claim to the insurance company and will be reimbursed at an agreed upon rate. If BILLED and PROCESSED correctly, there should be NO COST SHARING.
B. If there are a few providers in the directory, it is likely that those providers are in the system because of other credentials (e.g., a PA, NP, RN, MD that is credentialed with the insurance but also has a lactation consulting designation). In this case, the provider is responsible for understanding how the insurance company handles such breastfeeding claims and reimbursement will depend on the setting of the visit (e..g, home, office) and local state laws. These situations are usually difficult since the provider is likely to receive a very low reimbursement and may be tough to schedule an appointment with. In such cases, feel free to call the insurance company, tell them you have exhausted the in-network options and have no choice but to go out of network to find a provider.
C. If there are no providers in the network, you should tell your insurance company that you are going out of network and that they are responsible for covering the bill. In some cases, good insurance companies will go out of their way to find you a provider themselves. You will have to pay the fee to the provider and have the option to get reimbursed by your insurance company. Details on how to do this in step 2.
2. If you found yourself in situation 1A, consider yourself lucky. There are only a few insurance companies that provide good benefits for the mother, adequate reimbursement for the lactation consultant, and a clear and efficient process for payment. In the NY/NJ area, these insurances include Aetna and AmeriHealth.
Most people will find themselves in 1B or 1C situation. The 1B insurance plans include UnitedHealthcare and several others.
The 1C insurance plans (e.g., Horizon BCBS, Cigna) will reimburse you for the fee that you pay your lactation consultant – minus the travel fees. In order to get reimbursed, here’s what you should do:
- Ensure that your Lactation Consultant can provide you with an invoice that includes diagnosis codes and procedure codes. Consultants are NOT required to provide this, but really should.
- Ensure that your Lactation Consultant has experience with patients submitting claims on their own. If the invoice is coded incorrectly and the LC has no knowledge of coding, the headaches and appeals will not be worth your time.
- Once the Lactation Consultant provides an invoice, submit it immediately to the address on the back of your insurance card. Usually, your insurance company will also provide a reimbursement form on their website.
- The claim will either be paid in full, paid with cost-sharing (e.g., copayment, deductible, co-insurance), or denied.
- If you are reimbursed in full – congratulations! You and the LC have done a great job. Honestly, it shouldn’t be that difficult but at least you received the help you needed and were able to use your plan benefits.
- If the insurance company states that you have cost-sharing, call them to appeal. Explain that this is a breastfeeding claim and part of women’s preventive services, which should be covered at 100% in most cases. The diagnosis code here has to reflect the breastfeeding status (the code is Z39.1)
- If the insurance company denies your claim, have your lactation consultant provide input on why. Your first attempt should be to fix the errors and resubmit. If the claim gets denied again (and is coded correctly), you always have the option of getting your state insurance department involved. You can find the relevant contact by looking at the State’s website.
If this information is helpful, please comment and let me know. I am happy to provide more perspective on this in other posts. In the meantime, here’s proof (minus the HIPAA details) that claims get reimbursed (situation 1C).
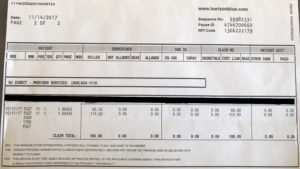
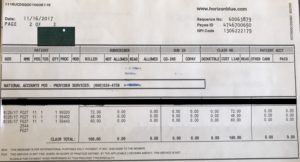
These were processed denied, appealed, and paid correctly eventually:
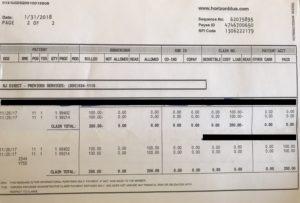
These were processed correctly immediately:
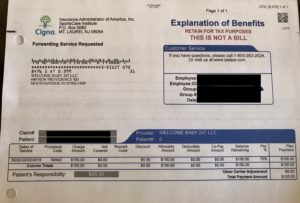
This one was paid but cost sharing should not have been applied: